Subscribe on your favorite player
Listen on Apple Podcasts Listen on Spotify Listen on Stitcher Listen on Google PodcastsInsomnia and Alzheimer's - Dr. David Holtzman & Dr. Kristine Yaffe
About This Episode
Families living with Alzheimer’s know that sleep patterns can change dramatically as the disease progresses. What does research tell us about Alzheimer’s, insomnia and other sleep conditions? What effect does sleep have on Alzheimer’s risk, and what solutions are there for better sleep, for those living with Alzheimer’s?
Press the 'Play' button under the image at left to hear the full discussion.
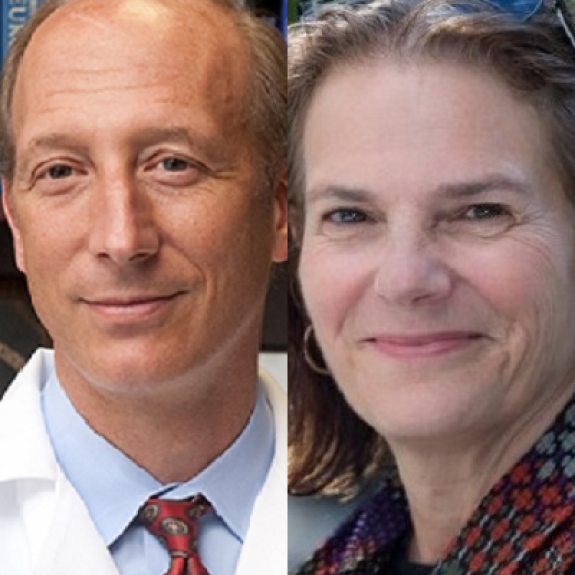
Host Meryl Comer spoke with two of the nation’s top researchers in this area:
- David Holtzman, MD, has led a number of studies linking sleep disorders to changes in the brain, as a potential marker for Alzheimer’s pathology and future risk of cognitive impairment. At Washington University in St. Louis, Dr. Holtzman is Chair of Neurology, Scientific Director of the Hope Center for Neurological Disorders, and Associate Director of the Knight Alzheimer’s Disease Research Center.
- Kristine Yaffe, MD, is an expert on populations studies of cognitive aging and modifiable risk factors for dementia, including sleep. She is Professor of Psychiatry, Neurology and Epidemiology and Chair and Vice Chair of Research in Psychiatry at the University of California, San Francisco. She is also Chief of Neuropsychiatry and Director of the Memory Disorders Clinic at San Francisco’s VA Medical Center.
As too many of us know, Alzheimer’s can lead to highly disrupted sleep—napping during the day, awake and wandering at night, and research shows that sleep is important for recent memories to fully form and that memory “playback” in sleep may help us remember things in the long term. But can poor sleep contribute to Alzheimer’s and other dementias?
Dr. Yaffe, Dr. Holtzman and others have shown that, in cognitively normal adults, sleep problems do seem to increase risk for dementia. Dr. Holtzman’s team has found that levels of amyloid and tau proteins, which build up in Alzheimer’s, increase acutely in the brain when sleep is disrupted. However, when deep sleep occurs, these proteins decrease within hours. In addition, research suggests that it’s not how many hours you sleep but how well. Poor quality of sleep seems to affect risk for Alzheimer’s and dementia more than sleep duration.
In mid- to late stages of dementia, more drastic changes in sleep tend to occur. These changes often mean a much greater level of care is needed. For family members trying to shift their loved one’s sleep cycle closer to normal, Dr. Yaffe and Dr. Holtzman offered these tips:
- Keep your loved one active during the day—exercise can promote better sleep.
- Try to establish and stick to a daily routine.
- Keep lights on during the day. Avoid lights, TVs or smartphones in the bedroom, especially at night.
- Keep the bedroom cool and quiet.
- Limit your loved one’s caffeine consumption in the afternoon and evening.
- Check to see if any of their medications’ side effects include sleep disruption.
- Ask their doctor about cognitive behavioral therapy for insomnia (CBT-I). CBT, which is used to improve mood or relieve anxiety, is also effective for improving sleep quality.
As for potential treatments that might minimize the effects of poor sleep on those with Alzheimer’s, a recent clinical trial just published by Merck found that Alzheimer’s patients slept better with a treatment called an orexin receptor antagonist. As Dr. Holtzman noted, we do not yet know whether this treatment has a functional benefit beyond improving sleep. However, he said, “It’s an area that’s worth exploring further.”
Major studies are building evidence for Alzheimer’s risk reduction through better sleep and other lifestyle changes. Dr. Yaffe is helping to lead the SMARRT prevention trial, which lets participants choose what risk factors they want to reduce in the study, and many participants want to work on sleep quality. Other studies, in people with mild cognitive impairment (MCI), are assessing whether improving sleep efficiency and quality can delay progression from MCI to Alzheimer’s.
Dr. Holtzman and Dr. Yaffe addressed a range of viewer questions:
- Fogginess from a few nights of bad sleep: In younger people, research suggests the fogginess may be transient if poor sleep doesn’t continue. A greater risk Alzheimer’s/dementia risk has been noted in older people with long-term sleep problems.
- Napping: If you did not sleep well, napping is helpful. However, for adults aged 70 and older, studies show that if you regularly get a good night’s sleep and still need a nap, it could signal a problem, including the beginnings of dementia. In cognitively normal older adults, those who are developing very early Alzheimer’s tend to nap more.
- Sleep medications: Some sleep medications may be helpful short-term but problematic over longer periods. Trying to improve your sleep is worthwhile, but non-pharmaceutical approaches are best.
- What can I expect in a clinical trial on Alzheimer’s and sleep: Study participants might keep a diary of their sleep patterns for a week or two and answer daily questions about their sleep. They may be given a wearable device, similar to a smartwatch, that tracks movement while sleeping. Other studies may connect wires to the participant to track sleep stages or detect apnea, but even this method is shifting to wearable devices that allow participation from home.
This Alzheimer’s Talk was generously supported by an independent grant from Merck.
To stay up to date on Alzheimer’s news, sign up here for our Alzheimer’s Daily newsletter.
